Welcome to episode 427 of The Whole View! This week, Stacy and Sarah look at different stomach ailments, what potentially causes them, and what role the gut microbiome plays. They explore the potential long-term effects these illnesses can have and explain how this can tie into osteoporosis.
If you enjoy the show, please review it on iTunes!
The Whole View, Episode 427: The Link Between IBS and Osteoporosis
Welcome back to episode 427 of the Whole View. (0:34)
Stacy shares that she’s the one who actually requested this topic.
Stacy says she has many people in her life with gut-related issues.
Yet she doesn’t really know the difference between IBS, IBD, Crohn’s, and Colitis.
She’s not sure how she’s gotten to this point. But she does know she needs to take a step forward in her knowledge base.
Stacy and Sarah talk about gut health on this show because of how important it is.
And just like the universe, the knowledge on this is ever-expanding.
Stacy believes that this topic is foundational to understanding gut health.
Sarah shares she’s been researching the gut microbiome for over six years.
When she decided to write a book about it, she thought it would be the same amount of information as in her other books.
However, she’s found that it changed her perspective on literally everything she and Stacy talk about.
Sarah thinks she’s finally at a place in her research where she finally has a handle on the vast amount of research there is out there.
Listener Question Regarding Osteoporosis
Sarah dives in with a listener question. (5:05)
“Sarah and Stacy- I am so inspired by your podcast. My husband and I have been listening for years. We binged them all initially, and now listen weekly while preparing dinners together. We have benefited greatly from your advice and recommended products. I have Sarah’s Paleo Approach and sleep books, we use our Joovv everyday, I switched us all to safer Beautycounter products from Stacy about two years ago. So thank you for making such a positive difference in our lives!
My mother was just diagnosed with full blown osteoporosis, notably in her right femur bone. Her bone test four years ago was healthy. My question is whether her struggles with IBS and gut health might have played a role in her diagnosis, and what could she do now to improve it?”
Stacy jokes about how much she loves nice, positive, complimentary questions.
She suggests that before they get into answering the question directly, they look at the root cause.
There is a reason that osteoporosis exists, and it’s something they’ve discussed on previous shows, as well as nutrient deficiencies.
This inevitably leads to IBS and other issues, and how that plays into nutrient deficiencies.
Stacy suggests they back and talk a bit about those other gut-related issues first.
Sarah agrees that explaining the issue is a lot like a spiderweb.
What Are The Differences?
Sarah goes back to Stacy’s questions at the beginning of the show, regarding the differences between IBS, IBD, Crohn’s, and ulcerative colitis. (7:53)
IBD stands for Inflammatory Bowel Disease, while IBS stands for Irritable Bowel Syndrome.
Crohn’s and ulcerative colitis are included under IBD.
What separates them is which part of the bowel is impacted by the autoimmune diseases.
Celiac disease is not characterized as an IBD due to its link with gluten as a trigger but is an autoimmune disease that causes inflammation in the bowel.
Sarah goes on to explain that IBS is a diagnosis of exclusion. It’s the label given once all other bowel issues are tested for and ruled out.
Sarah expresses how frustrating IBS can be because it’s such a catch-all.
You go in with an irritable gut, and when you test negative for all the things they can test for, they go, “congratulations, you have an irritable gut.
Sarah shares her personal story of getting diagnosed with IBS-C.
It can be classified as diarrhea-predominant (IBS-D), constipation-predominant (IBS-C), with alternating stool pattern (IBS-A). People can experience:
- Abdominal pain, cramping, or discomfort
- Gastrointestinal: change in bowel habits, constipation, diarrhea, inability to empty bowels, indigestion, nausea, passing excessive amounts of gas, or urgent need to defecate
- Also common: anxiety, depression, discomfort, loss of appetite, or symptoms alleviated by defecation
Stacy asks Sarah whether the depression she spoke of could be caused directly by gut health issues or as a side effect of the symptoms’ discomfort.
Sarah shares some of the research that emerged in recent years that points to possible causes.
Possible Causes of IBS
IBS might not be just one thing, but possibly a bunch of different things that all get a diagnosis of exclusion label. (16:40)
Sarah goes on to explain that the research in the last 10 years has pointed to two main possible causes that are probably closely related.
And are also a probable link to IBS and other health issues, including mental health.
Food Intolerance
Sarah says one of the most common factors causing IBS patients’ symptoms is a food intolerance, with some studies reporting it in up to 89% of their patients.
Patients with IBS understand that specific types of food trigger their symptoms: usually.
These include legumes, vegetables, lactose-containing foods, fatty foods, stone fruits, and artificial sweeteners.
This includes food allergies and is studied via blood tests and trial and error removal.
Another way this is often studied and combated is by putting people on low FODMAP and gluten-free diets, which have shown greater even results.
Stacy takes a moment to underline the fact that there are medications out there that don’t even have the 70% improvement rate that these dietary changes do.
Stacy wonders how many doctors are prescribing low FODMAP diets.
Sarah shares that she doesn’t have those numbers, but she can say no one talked diet with her through her IBS experience.
Stacy shares when you struggle with these symptoms for so long, you don’t really know what “normal” is.
Often, doctors aren’t given information and description that would prove helpful because nothing is out of the ordinary to the patient.
Sarah explains that the issue here is that IBS is kind of a useless diagnosis because there are so many shades of it. 24:57
Sarah thinks that one of the things adding to this percentage of success is that many people who see improvement by going on a low FODMAP diet have never tried changing their diets before that point.
She said that the reason so many people might be responding to a FODMAP diet is that they’re eliminating wheat from their diets.
FODMAP intolerance is most typically caused by gut dysbiosis, which co-occurs (chicken vs egg) with stress, poor digestion, leaky gut.
Gut Dysbiosis
This growing body of literature shows that with IBS, there is a loss of bacterial diversity, the establishment of problematic and opportunistic pathogens-like species in the gut, a lack of probiotic species, and many other things we know are associated with health conditions in general. (26:24)
That kind of imbalance in the microbial community in the gut by itself can drive IBS symptoms but can also explain the reactions we see in dietary interventions.
About 60% of the inputs that determine what bacteria are growing in our digestive tract is diet.
And the other 40% is lifestyle, exposures (environmental toxins, supplements, drugs, hormones), stress, sleep, etc.
Sarah explains that the gut microbiome’s composition can shift dramatically in just a few days or weeks, depending on what the “starting microbiome” looks like.
What happens in the gut microbiome when diet changes are made is it’s finding a new equilibrium.
This eventually reaches stability in about six months.
Unknown vitamin deficiencies (such as Vitamin D), lifestyle factors, and heavy metal or pesticide exposure are also known to drive gut dysbiosis.
Sarah explains that this means you might have a gut-bacterial-profile that produces a lot more gas when you consume gluten or a FODMAP-rich food.
Sarah sums up that FODMAP intolerance is basically a measurement of gut dysbiosis.
The Unrealized Impact
Stacy shares how she’s recently been seeing a lot of people talk about bloating as being “normal” right now. (30:38)
She believes that just because it’s common doesn’t mean it’s normal.
And that seeing 75% of people having symptom reduction just from going gluten-free is brain exploding results.
Stacy thinks that there’s a vast majority of people who aren’t talking about it with their doctors, nor are they seeking out functional medicine practitioners and wholistic nutritionists to help.
Most people who are doing that are kind of already making dietary changes.
Gut Dysbiosis As An Indicator
Stacy tries to wrap her brain around how many people could be living happier lives, healthier lives, just by making this change. (32:18)
She explains that that’s the really important part, and gets us back to the question at hand because it isn’t just about discomfort.
This really can cause, especially long-term, serious health problems.
Sarah explains that though it’s not the only indicator, you’re not going to experience IBS if you have a completely healthy gut microbiome. It’s just not something that happens.
The research actually links gut dysbiosis with every chronic illness.
It’s easy to think of it in terms of GI issues but is, in fact, linked to diabetes, obesity, cardiovascular disease, cancer, mental health disorders, autoimmune diseases, asthma, and osteoporosis.
Sarah also explains that it’s linked in a couple of different ways.
Gut bacteria are very important modulators of our immune function and control how our immune system responds to stimuli. Gut bacteria also controls our gut-barrier.
Sarah also goes into the connection between leaky gut and the gut microbiome.
This is because the microbiome is controlling how leaky the gut barrier is. So to fix one, you need to fix the other.
Gut Microbiome and Osteoporosis
If your gut barrier is not working properly, you are not absorbing nutrients properly, such as calcium. (34:41)
Sarah explains that even after we’re done growing, our bones are being constantly broken down and built back up.
This is done in equilibrium, and it’s what gives us bone structure.
We lose that balance as we age, but also through nutritional and lifestyle imbalances.
Sarah also explains the more diversity you have in your gut, the more density you have.
The less bone density you have, the greater your chance of having and/or developing osteoporosis.
The Question of Obesity
Stacy asks if we’re able to call out the issue of obesity for a moment. And whether it’s contributes to an unhealthy microbiome, or rather a result of, similar to osteoporosis. (38:40)
Sarah explains a phenomenon of weight gain regarding the obesity microbiome and how it drives the increased health risks of obesity.
She tells us that the takeaway form the research done is that it’s not so much the weight that indicates health status, but the healthy choices.
For more information on this topic, check out Episode 421: Body Image.
Stacy takes a minute to remind listeners that what is said on this show is not meant to make anyone feel guilt or shame or things like health and/or weight.
She explains that what matters is you are doing the best you can do for your health with the information available to you.
Adding stress or anxiety does not do anything to help you reach a healthier you.
Fixing IBS
Sarah takes a few minutes to run through a quick recap of information covered in previous shows due to these topics’ tendency to overlap.
She also goes over a few action-points covered in her Gut Guidebook.
Sarah notes that low-FODMAPS can make dysbiosis worse, even if it improves symptoms, which is why she personally doesn’t recommend this diet.
She reminds listeners that more people responded to gluten-free in IBS studies than low-FODMAP. And that wheat is eliminated on low-FODMAP diets as well.
But many gut-microbiome-beneficial foods that might not be contributing to IBS symptoms are cut out as well, putting you at a disadvantage.
Stacy and Sarah discuss the benefits of low-FODMAP diets as a temporary treatment.
Notable Episodes for More Information
A high variety of veggies, fruit, mushrooms, nuts, and seeds are very important to a healthy gut microbiome.
If anything increases symptoms, be sure to back off of it and add it back in gradually.
Try cooked veggies, purees, smoothies for IBS-D, and try raw salads for IBS-C symptoms.
This is something Stacy and Sarah have covered in many other episodes:
Stacy and Sarah discussed the benefits of increasing fish intake and/or take fish oil in Episode 415: Fish oil, Healthy or not? And the importance of hydration in Episode 406: Got Water?
In Episode 414: Best Cooking Fats for Gut Health, Sarah and Stacy talked about EVOO as go-to fat.
Probiotic foods (sauerkraut, kombucha, kefir), discussed in Episode 329: The Link Between Carb Intolerance & Gut Health, are also great avenues to explore.
Sarah reminds listeners to get enough sleep and do so on a consistent schedule.
Manage stress is also important, as discussed in Episode 397: Practical Tips for the Sleep Stress Cycle.
Sarah also recommends increasing activity (but avoid overtraining), especially walking.
She explains that microorganisms operate on a cycle, so the best practice is to eat distinct meals, with 12-14 hours fast overnight.
What About Milk and Dairy?
Stacy jokes that what Sarah is really saying is we can solve many of these issues by drinking large glasses of fortified cows milk.
She reminds listeners, however, many milk-based products in stores have a lot of additives.
She goes on to say that veggies are not only adding the nutrition you need, but also fiber, antioxidants, and many of the anti-inflammatory properties the body needs.
Stacy tells the audience that that’s why milk isn’t on their list, but is commonly associated with other lists regarding bone health and osteoporosis.
Sarah jokes about dropping some mind blowing science on us.
She tells us that studies show the strongest dietary factor contributing to healthy bone is fruit and vegetable intact. And that it’s much strong than results from dairy intake.
How Fruits and Vegetables Help
Sarah cites that the calcium in fruits and vegetables are actually easier for our bodies to absorb:
“Not only do fruits, vegetables, nuts, seeds, and seafood contain substantial amounts of calcium, but there is scientific evidence that we absorb more calcium from cruciferous vegetables (like kale) than we do from dairy.”
Cruciferous vegetables (like kale, cabbage, broccoli, collard greens, and turnip greens) may be the best source of dietary calcium.
Several studies show that fruit and vegetable intake correlates much more strongly with bone health than dairy intake.
The scientific evidence is mixed on dairy and bone health.
Some studies indicating that higher dairy consumption may increase the risk of fractures and osteoporosis.
Sarah attributes this to the critical role the gut microbiome plays throughout our entire body,
Yes, to prevent osteoporosis and look after your bones, eat your veggies!
Bone Health Nutrients
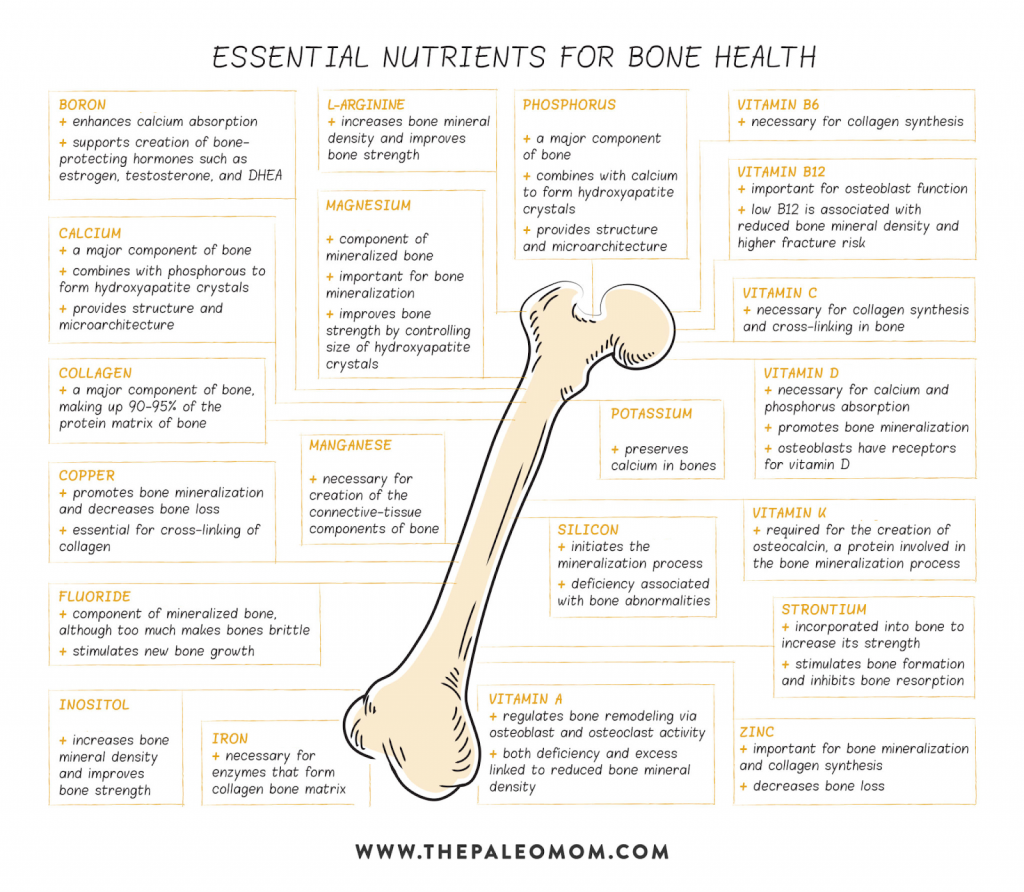
There’s at least twenty micronutrients that are essential for bone health.
Bone is composed of a mixture of minerals (calcium, phosphorous, magnesium, sodium and potassium, mainly) deposited around a protein matrix that acts as a scaffold.
It’s the combination of inorganic (minerals) and organic (protein) materials that provide bone with both strength and flexibility.
About 65% of bone tissue is minerals, chiefly calcium and phosphorous.
The remaining 35% a protein matrix, 90 to 95% of which is type I collagen.
Once fully grown, bones are constantly being remodeled at an equilibrium that decreases as we age.
As bone density drops, we see the development of osteoporosis.
Sarah also tells listeners that maintaining insulin sensitivity is key to regulating bone remodeling.
Bone Health and Osteoporosis
- The major protein in bone is collagen. Vitamin C, copper and zinc are essential for collagen formation
- Calcium, phosphorus, magnesium, potassium
- Fat-soluble vitamins (A, D, and K2 in particular) are essential regulators in bone mineralization.
- vitamin D status influences calcium absorption. So, testing to make sure your serum vitamin D levels are in the functional range (50 to 70 ng/mL is probably optimal) and supplementing accordingly is essential.
Veggies for the win!
Final Thoughts
Stacy returns to the listener’s question from the beginning of the show about whether or not a struggle with IBS could later develop osteoporosis. (1:09:02)
She says, looking back at all the science, the answer is yes.
Stacy suggests she now follow protocol for improving gut health.
She also says to be mindful of short-term FODMAP diet. And potentially conferring with a holistic approach.
Stacy explains that when you’re experiencing health issues with a certain part of your body, one of the best things you can do is consume animal parts of that body.
For example, bone broth contains many of the nutrients needed to support bone.
Stacy recommends replacing soup and stew recipes that call for vegetable broth with bone broth.
If you’re interested in learning more about bone broth, check out Episode 313.
Stacy says one of the most important things to take away from this episode is nourishing your bones with the nutrients you need.
Stacy thanks listeners for spending this time with them.
She reminds us that there a show on collagen on the docket (as soon as Sarah can get her head wrapped around the science).
If you have follow-up questions on anything covered in this episode, Stacy and Sarah invite you to reach out in any way.
Stacy adds that Patreon is the fastest and easiest way to reach them.
So if you haven’t joined the Patreon family yet, be sure to pop on over. Check out the bonus content while you’re there!
Thanks so much for listening!