Welcome to episode 468 of The Whole View! This week, Stacy and Dr. Sarah break down the science behind the Delta Covid-19 variant, how it’s different, and how it impacts vaccine effectiveness.
If you enjoy the show, please review it on iTunes!
The Whole View, Episode 468: The Delta Covid-19 Variant
Welcome back to episode 468! (0:28)
Stacy and Dr. Sarah have several episodes covering the topic of Covid. So for any new listeners or listeners looking for a quick refresh.
We also remind listeners that Stacy and Dr. Sarah are not medical professionals. So be sure to check with your healthcare provider before taking any action.
Episode 394: Covid-19 addresses all things coronavirus, also known as covid-19, including is this disease, the symptoms, how it’s spread, and what we can do to reduce our risk of infection.
Episode 397: Covid-19 FAQ answers listeners’ questions on covid-19, what the latest data says on what to expect, the biggest risk factors, ways to minimize our risk or symptoms if we get sick.
In Episode 401: Covid-19 NEW FAQ. Stacy and Dr. Sarah answer even more listeners’ questions about vaccine development, non-medical grade face masks, rapid testing, and reinfection.
Episode 412: Covid-19 FAQ, Part 3 covers how quarantine impacts our gut microbiome, if healthy habits and supplements can lower our risk of getting sick, and if science has advanced on what we know about antibodies and immunity.
Episode 425: Covid-19 FAQ Part 4 focuses on the long-term impacts of covid-19, the validity of reinfection cases, and the science behind covid-19 reactivation.
Episodes on Covid-19 Vaccine
Episode 440: Covid-19 Vaccines Part 1 – mRNA Vaccine Technology examines the history of vaccines, the very real statistics on vaccine-induced injury, and the advances that led to mRNA vaccine technology.
Episode 441: Covid-19 Vaccines Part 2 – Pfizer/BioNTech vs. Moderna looks at the safety and efficacy data from the phase 2/3 clinical trials for both the Pfizer/BioNTech and the Moderna covid-19 vaccines.
In Episode 443: Covid-19 Vaccines Part 3 – FAQs, Stacy and Dr. Sarah answer listener FAQs, including concerns about adverse events including autoimmune disease, fertility, and the current state of evidence in terms of safety concerns for pregnancy and children.
Episode 444: Covid-19 Vaccines Part 4 – Myth Busing talks about the myths surrounding antibody-enhanced infection, the for-profit argument, mRNA vs. DNA, traces of controversial tissue cells, and hidden foreign bodies. Stacy and Dr. Sarah also cover who should wait to get the vaccine and vaccine aftercare.
Episode 454: J&J and AstraZeneca Covid-19 Vaccines looks at how adenovirus vaccines work and the safety and efficacy data from the phase 2/3 clinical trials for both the Johnson & Johnson & Janssen and the AstraZeneca/Oxford University vaccines. Stacy and Sarah do a deep dive into immune thrombotic thrombocytopenia and what the news is reporting as a rare type of blood clot.
Episode 455: Covid-19 Vaccines – Real World Data and Updated Studies discusses new studies in pregnant and lactating women, breakthrough infections, updated vaccine studies for the second dose, variants of concern coverage by vaccines, monoclonal antibody therapies, and menstruation irregularities.
Dr. Sarah also has a great summary article on vaccines and face mask science.
The Delta Covid-19 Variant
The Delta variant, also called B.1.617.2, was first identified in India in December 2020. (5:48)
It is called “Delta” due to a Greek alphabet naming system to avoid stigmatizing names based on countries where variants are identified. Several technical naming systems describe either lineage or amino acid differences, which are confusing and don’t mean much for the general population.
The only variants that get a Greek letter and those deemed “variants of concern.” These transmissible variants cause more severe illness, cause more death, or evade immune responses from vaccines or previous natural infections.
The Delta variant was the fourth identified variant of concern. And Delta is the Greek equivalent of the letter D- the fourth of the alphabet.
Delta Covid-19 Varient Mutations
Dr. Sarah reminds listeners that the novel coronavirus doesn’t mutate very quickly compared to other viruses like influenza. But because it’s novel (humans have never encountered it before) and has spread globally, it has had many opportunities to mutate.
We’re racing the virus and trying to achieve herd immunity before the virus mutates in a way that allows it to evade the immune protection we get from vaccination or natural infection.
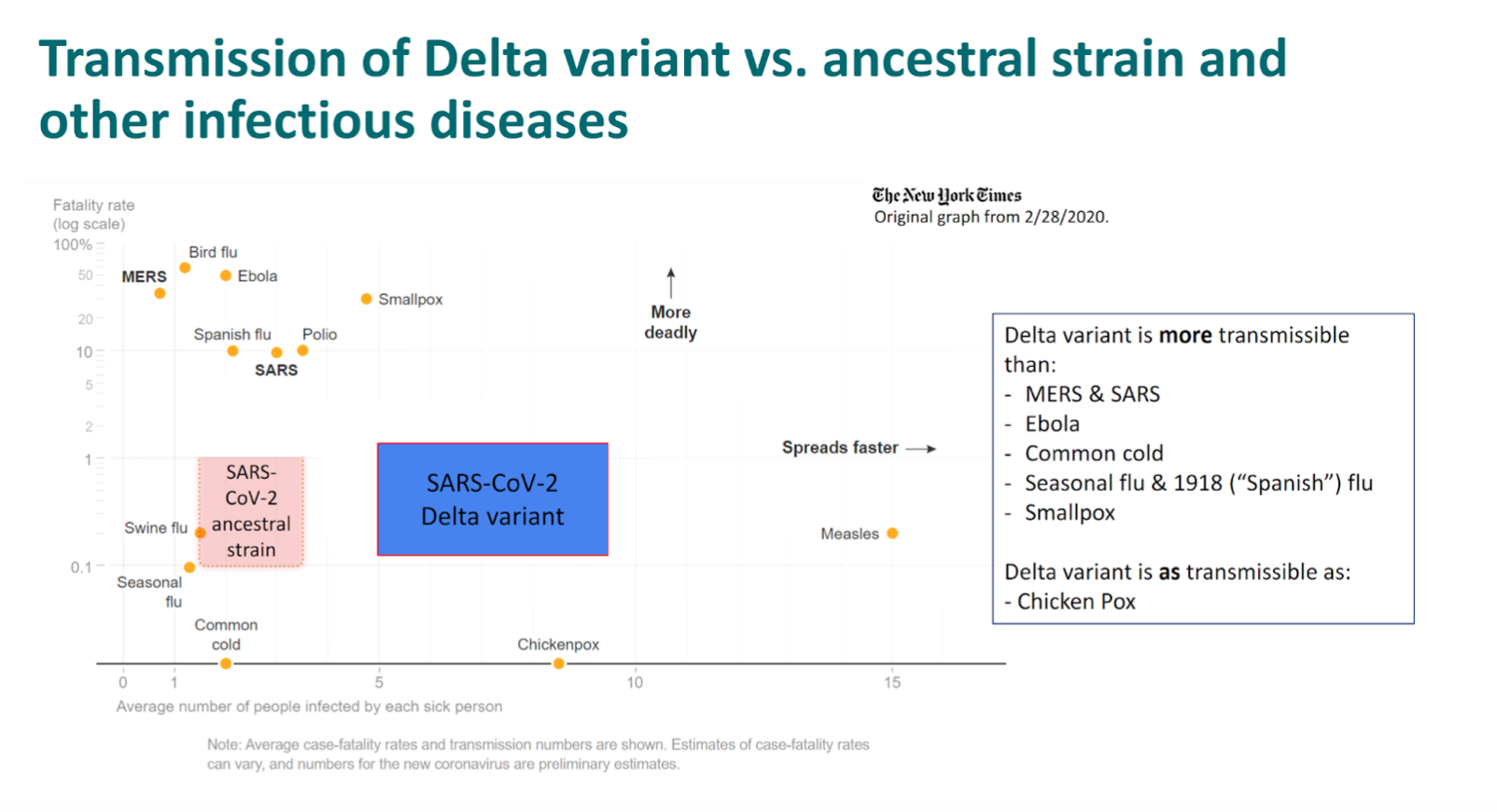
Delta is not the worst-case scenario, and we are not back to square one. The vaccines are still extremely effective against the Delta Covid-19 variant. However, it’s about as contagious as chickenpox and more than double the original virus.
The Delta Covid-19 variant doesn’t have the N501Y spike mutation found in the alpha, beta, and gamma variants, which enabled them to invade cells more successfully than the original virus.
Delta also lacks the E484K mutation, which has made the gamma variant so worrisome. This genetic change allows the virus to spread even among vaccinated people, so the vaccines do fairly well against Delta compared to other VOCs.
Bad News About The Delta Covid-19 Variant
Like all the identified variants in circulation, Delta contains a spike mutation called D614G, sometimes known as “Doug,” which became ubiquitous last year. (14:39)
Scientists think Doug increases the density of spike protein on the surface of viral particles and makes it easier for the virus to enter cells.
Delta also has a spike mutation called P681R, which closely resembles a mutation in the alpha variant that appears to produce higher viral loads in patients.
People infected with Delta have 1,000 times more virus in their respiratory tract, making them more likely to spread the virus when they sneeze, cough, or talk.
The P681R mutation, also found in the kappa variant, is located at the beginning of a part of the genome called the furin cleavage site. Furin is a naturally occurring human enzyme that gets hijacked by the coronavirus, which uses it to slice the spike protein into the optimal shape for entering the cell. The new mutation makes that sculpting more efficient.
Experiments suggest that the L452R mutation, which also affects the receptor-binding domain, prevents antibodies from neutralizing the virus.
The mutation is structurally located in the interaction region with human receptor ACE2 and thought to affect affinity with human cells and influence viral infectivity.
Fusing with human cells allows the coronavirus to dump its genetic material into those cells.
It’s the combination of these mutations that makes Delta so much more contagious than any other VOC, giving it a competitive advantage, which is why it’s the dominant strain globally.
- Sarah’s Sources
- khn.org/news/article/unraveling-the-mysterious-mutations-that-make-delta-the-most-transmissible-covid-virus-yet/
- asm.org/Articles/2021/July/How-Dangerous-is-the-Delta-Variant-B-1-617-2
- pubmed.ncbi.nlm.nih.gov/33558493/
- virological.org/t/viral-infection-and-transmission-in-a-large-well-traced-outbreak-caused-by-the-delta-sars-cov-2-variant/724
- covariants.org/variants/21A.Delta
- biorxiv.org/content/10.1101/2021.03.28.437369v3
Delta Covid-19 Variant Infection Dynamics
When the pandemic began, people spread the original coronavirus to an average of two or three people. (19:45)
Today, people infected with Delta infect six people, on average, a similar R0 to chickenpox and higher than previous VOCs, other coronaviruses, influenza, common cold virus, polio, ebola, Spanish flu, etc.
The Delta Covid-19 Variant has an incubation period of four days rather than six, making people contagious sooner.
Delta is also contagious for longer. The average duration you’re contagious with Delta is 18 days, but it was 13 days for the original virus.
Sarah also recommends this paper comparing the different Covid-19 variants.
Delta Symptoms
According to surveys conducted in the U.K., where Delta accounts for ~90% of current COVID-19 cases, the Delta Covid-19 Variant symptoms tend to be a little different than other strains. (23:00)
But that does not necessarily mean the associated symptoms are more severe.
Fever, headache, sore throat, and runny nose are common. However, cough and loss of smell are less so compared to the original virus.
Other reports link Delta to more serious symptoms, including hearing impairment, severe gastrointestinal issues, and blood clots leading to tissue death and gangrene.
This is really the perfect storm of transmissibility. It’s contagious earlier and for longer, with a higher viral load (especially important the day before symptoms start) and symptoms that someone might not recognize as covid-19.
As a result, Delta has a major competitive advantage over all other variants of covid-19. It’s now in at least 132 countries!
Severity & Mortality Risk
Research is ongoing to determine if Delta infection is associated with increased hospitalization and death. (30:01)
Being more contagious and spreading so quickly will cause more hospitalization and death. However, a couple of earlier studies also show a higher risk to unvaccinated people than the original coronavirus.
One early study assessing the risk of hospital admission in Scotland reported that hospitalization is twice as likely in unvaccinated individuals with Delta than in unvaccinated individuals with alpha.
- The Cox regression analysis for time to hospital admission found that S gene-positive cases were associated with an increased risk of COVID-19 hospital admission.
- Hazard ratio (H.R.) was 1·85 (95% CI 1·39–2·47) when compared to S gene-negative cases after adjusting for age, sex, deprivation, temporal trend, and comorbidities.
- A greater number of COVID-19 relevant comorbidities increased the risk of COVID-19 hospital admission (appendix p 3).
Further Studies
Another study out of Singapore showed, after adjusting for age and gender, B.1.617.2 infection was associated with higher odds of oxygen requirement, ICU admission, or death (adjusted odds ratio (aOR) 4.90, [95% CI 1.43-30.78].
- 157 patients with VOCs were admitted to their centre.
- After adjusting for age, gender, comorbidities, and vaccination, aOR for pneumonia with B.1.617.2 was 1.88 [95% CI 0·95-3·76]) compared with wildtype.
- B.1.617.2 was associated with significantly lower PCR Ct values and a significantly longer duration of Ct value ≤30 (estimated median duration 18 days for B.1.617.2, 13 days for wildtype).
- Vaccine breakthrough cases were less severe.
And study out of Canada compared to wildtype showed increases with Delta variant were more pronounced.
According to the CDC, people ages 18 to 49 make up the largest demographic of hospitalized people due to COVID-19.
However, that’s attributed to lower vaccination rates, not (at least as we know) because Delta is more dangerous than other variants to young people.
Now on to some good news!
Vaccine Efficacy
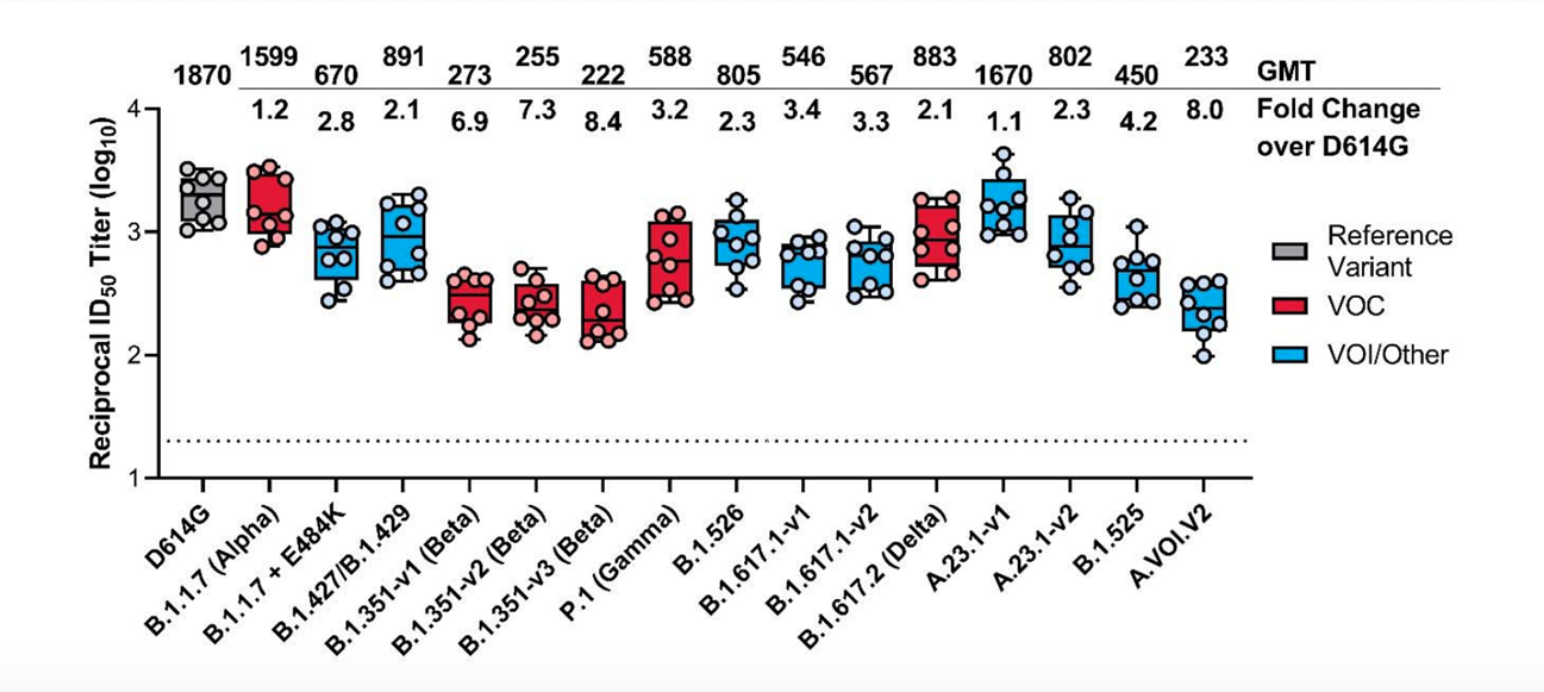
In vitro studies show that the antibodies we make when vaccinated neutralize Delta more effectively than several of the other variants of concern. (39:42)
Those variants include Beta (B.1.351 South Africa) and Gamma (P1 Brazil), although not quite as well as Alpha (B.1.1.7 UK)
And, real-world data shows the vaccines are doing their job!
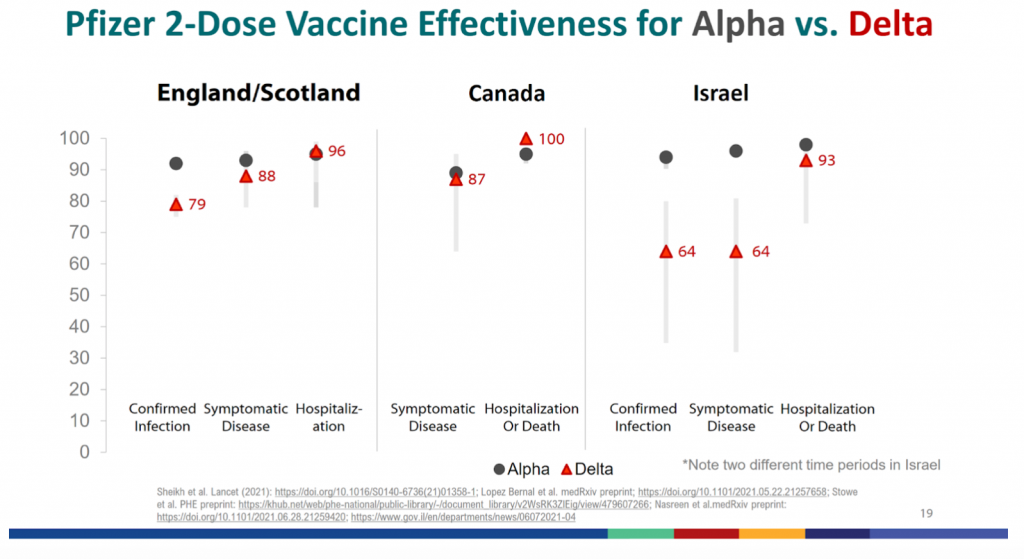
U.K. Study in the New England Journal of Medicine took a test-negative, case-control design to estimate vaccine effectiveness against symptomatic disease caused by the Delta variant, compared to alpha.
They reported an 88% efficacy against Delta after 2 doses of mRNA vaccine, but only 30.7% efficacy after 1 dose.
Two doses of the Pfizer-BioNTech vaccine protect 94% of people from any symptomatic infection by the alpha variant, compared with 88% against the delta variant. And Two doses of the AstraZeneca vaccine protect 75% of people from alpha and 67% from Delta.
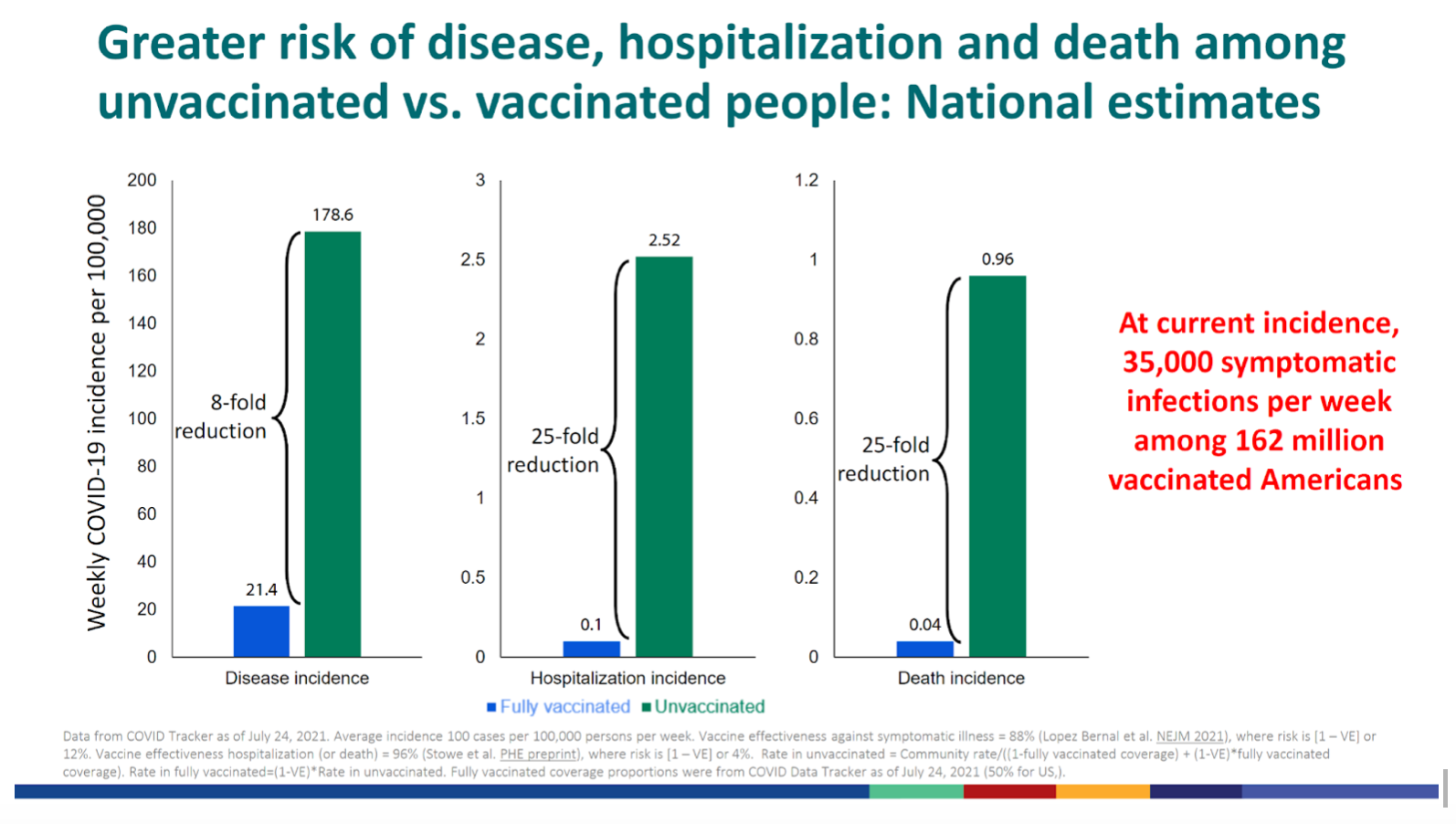
All-in-all, vaccines protect 3-fold reduction against testing positive, 8-fold reduction against symptomatic disease, and 25-fold reduction against hospitalization and death.
The United States
In the USA, an average of 97% of hospitalizations and 99.5% of covid-19 deaths are among unvaccinated but varies from state to state.
The reported share of COVID-19 cases among those not fully vaccinated ranged from 92.02% in Oklahoma to 99.85% in Connecticut.
The share of hospitalizations among those with COVID-19 who are not fully vaccinated ranged from 95.02% in Alaska to 99.93% in New Jersey. Dr. Sarah notes hospitalization may or may not have been due to COVID-19.
The share of deaths among people with COVID-19 who are not fully vaccinated ranged from 96.91% in Montana to 99.91% in New Jersey. (Note: Deaths may or may not have been due to COVID-19.)
England
In England, nearly 90% of the adult population has had at least one dose, and over 70% of adults have had both doses. But, there’s a higher level of Astrazeneca vaccine used. (45:15)
Public Health England said on Friday that of 3,692 people hospitalized in Britain with the Delta variant, 58.3% were unvaccinated, and 22.8% were fully vaccinated.
The percentage of hospitalized people who are fully vaccinated is expected to increase with the percentage of the vaccinated population while there are high spread levels.
We can clearly see the benefit of the vaccines comparing high-vaccination rate states to low. On average in the USA:
- Hospitalizations among states <50% are vaccinated is 14.4 per 100,000
- Hospitalizations among states >50% are vaccinated is 4.9 per 100,000
- Daily cases rate over past week <50% is 23.7 per 100,000
- Daily cases rate over past week >50% is 9.3 per 100,000
- Average daily deaths <50% is 129 per 1 million
- Average daily deaths >50% is 55 per 1 millio
The takeaway: the vaccines work! They are doing their job keeping people out of the hospital and alive.
Breakthrough Infections
So what about the data that led the CDC to recommend that everyone go back to wearing masks indoors? Well, no vaccine is perfect. (1:00:10)
A breakthrough inflection is an infection that happens after you’re fully vaccinated, which is 2 weeks after your second shot.
Mild to moderate disease with covid-19 is much worse than most of the infections we’ve come to live (like the flu). So it may feel severe even though clinically it would be classified as mild.
The main thing is that even if you do get a breakthrough infection, the vast vast vast majority of people are protected from a severe disease requiring hospitalization, a critical disease requiring ICU, and death.
The rate of breakthrough infections with the Delta Covid-19 variant is higher than other variants. It’s as high as 36% and prevents 64% of infections.
But data is still being collected in various regions, so that number may change as we learn more.
Why It’s Important
You may be able to transmit disease with a breakthrough infection. And this is why the CDC wants us all to mask up again.
Breakthrough cases reported to national passive surveillance have lower Ct values by 3 cycles (~10-fold increase in viral load) for Delta (Ct=18, n=19) compared with Alpha (Ct=21, n=207) and other lineages (Ct=21, n=251).
With alpha, a vaccinated person with a breakthrough infection still had a much lower chance of transmitting. However, this might not be the same with Delta.
Barnstable County, MA, outbreak: there’s no difference in mean Ct values in vaccinated and unvaccinated cases [median among vaccinated (n=80): 21.9; unvaccinated(n=65): 21.5].
Dr. Sarah reminds listeners that viral load is not the same as transmissibility. It’s completely possible that most of that virus is not viable, but…
Mounting data showing reduced (but still substantial) transmission from breakthrough infections during time range that captures the shift from alpha being dominant strain to Delta
Data from Israel
Studies show that vaccines reduce the spread of SARS-CoV-2 by more than 80%, but the Delta variant is creating fresh uncertainty.
The first study, co-authored by researchers in Israel and France, looked at transmission in 210 households of infected people who worked at Israel’s largest hospital, the Sheba Medical Center near Tel Aviv.
The data come from between December 2020 and April 2021: a time when a massive vaccination drive in Israel was competing with a surge in cases driven by alpha.
The second study, co-authored by researchers in Israel and the United States, was based on a retrospective analysis of data from about 66,000 multiperson households with at least one infected member.
Both studies found that two doses of the Pfizer–BioNTech vaccine were 81% effective at preventing infections.
Those who did get infected were also less likely to pass the infection to household members than were unvaccinated individuals.
The first study saw a drop of 78%, and the second 41%, in reduction of infectiousness, with the large difference in numbers perhaps explained by the fact that the estimates are based on a very small number of vaccinated people who were infected and then infected others.
Further Reading:
- https://www.medrxiv.org/content/10.1101/2021.07.12.21260377v1
- https://www.medrxiv.org/content/10.1101/2021.07.13.21260393v1
Data from England
The results in Israel correspond well with studies conducted elsewhere.
One analysis of some 365,000 households in the United Kingdom, published on 23 June, estimated that individuals infected with SARS-CoV-2 were 40–50% less likely to spread the infection if they had received at least one dose of the Pfizer–BioNTech vaccine.
Or if they’d received the vaccine developed by the University of Oxford, U.K., and pharmaceutical company AstraZeneca, based in Cambridge, UK, at least three weeks previously.
Further reading:
Data from Finland
A study from Finland, posted as a preprint on 10 July, found that spouses of infected healthcare workers who had received a single dose of the Pfizer–BioNTech vaccine or that produced by Moderna in Cambridge, Massachusetts, were 43% less likely to get infected than were spouses of unvaccinated health workers.
Further Reading:
What It All Means
There’s no delta-specific data on the transmissibility of breakthrough infections. But the combo of higher viral load plus as little as a 40% reduced transmissibility for breakthrough infections, plus higher breakthrough infection rate, plus skyrocketing cases. All make a solid argument to mask up!
Masking up protects us individually from a breakthrough infection, even if it’s mild, protects anyone we live with who is not vaccinated, and reduces the spread of covid-19 in the community.
Myth Busting: Delta Covid-19 Variant
There’s misinformation being spread that these stats are all skewed because hospitals aren’t testing people who say they’ve been vaccinated or, if sick, you assume you didn’t get Covid-19. (1:07:01)
Another thing to consider is long-covid. With breakthrough infections, your chances are much lower but non-zero.
At the largest medical center in Israel, they identified breakthrough infections by performing extensive evaluations of symptomatic healthcare workers (including mild symptoms) or had known infection exposure.
Among 1497 fully vaccinated health care workers for whom RT-PCR data were available, 39 SARS-CoV-2 breakthrough infections were documented.
Neutralizing antibody titers in case patients during the peri-infection period were lower than those in matched uninfected controls (case-to-control ratio, 0.361; 95% confidence interval, 0.165 to 0.787).
Higher peri-infection neutralizing antibody titers were associated with lower infectivity (higher Ct values).
67% of cases were mild and 33% of were asymptomatic, although 19% had persistent symptoms (>6 weeks).
The B.1.1.7 (alpha) variant was found in 85% of samples tested.
A total of 74% of case-patients had a high viral load (Ct value, <30) at some point during their infection; however, of these patients, only 17 (59%) had a positive result on concurrent Ag-RDT. No secondary infections were documented.
Note: long-covid (6 week definition) is more like 30% in unvaccinated, and this is 19% of the 3% breakthrough infection rate in a population with a very high risk of exposure.
Will We Need Boosters?
Boosters are likely coming sometime in the next 6 months to a year. (1:20:01)
Older and immunocompromised adults will be prioritized since there’s also evidence these people have lower vaccine efficacy to begin with (still awesome in the grand scheme of things, but a booster could make it better).
Data shows 80% immunity against SARS-CoV-2 infection ≥7 days after 2nd dose of mRNA vaccine among people with IBD on immunosuppressive medication.
In addition, data shows 59% decrease in COVID-19 hospitalization among immunocompromised ≥14 days after 2nd dose of mRNA vaccine vs. 91% (CI 86-95%) without immune compromise.
The effectiveness of Pfizer’s COVID-19 shot can drop to 83.7% within four to six months after getting the second dose of its vaccine. This is the latest indication that vaccine-induced immunity to the virus can wane, and some kind of boost may be necessary for the future.
New research published as a preprint indicates that the Pfizer Inc. shot provides 96.2% protection for the first two months, 90.1% effectiveness between the second and fourth months, and between 83.7% of protection for the fourth, fifth, and six months. This data was before Delta emerged.
Variants Might Be A Factor
Pfizer recently shared preliminary data from lab tests that suggests a third dose of its shot is associated with a five-fold increase in antibodies in people between the ages of 18 to 55 after their second dose; for those between 65 and 85, it’s 11-fold.
Dr. Sarah recommends this article for more information.
Both Pfizer and Moderna are working on boosters that will give better coverage against the variants of concern that have emerged.
There’s a question for vaccine equity here too.
Only 14.4% of the world population is fully vaccinated. However, 28% of that has received at least one dose of a vaccine, with 4.07 billion doses given globally.
Only 1.1% of people in low-income countries have received at least one dose.
Remember, Delta originated from a surge in infections in India where a fire in a factory delayed vaccine rollout. So, until the world is protected, this isn’t over.
Steps to Take
Stopping transmission is the key to controlling variants.
WHO has said we are only a few mutations away from going back to ground zero. But some infectious disease experts think Delta is the worst it will get because any mutation that makes it evade the immune system (or more deadly) will reduce transmissibility, like mutation tug of war.
Either way, getting infection rates back down will save lives. If you haven’t yet, get vaccinated ASAP.
There are many rumors around, which is why we did six shows explaining how the vaccines work and answering FAQs, and busting myths.
It’s time to go back to universal masking, especially indoors but also in crowded outdoor areas.
It’d also be worth mentioning that there are so many awesome innovations out there to make masks more comfortable. Social distancing and avoiding crowds when possible is also recommended.
Additional Citations
- context-cdn.washingtonpost.com/notes/prod/default/documents/8a726408-07bd-46bd-a945-3af0ae2f3c37/note/57c98604-3b54-44f0-8b44-b148d8f75165.#page=1
- cdc.gov/mmwr/volumes/70/wr/mm7031e2.htm?s_cid=mm7031e2_w
- nature.com/articles/d41586-021-01986-w
- nature.com/articles/d41586-021-02054-z
- medrxiv.org/content/10.1101/2021.07.28.21261295v1
Final Thoughts
As long as there are places where transition rates of Covid are high, we’re at risk for virus variants. So this pandemic isn’t over until vaccines are available everywhere.
We know we can do here in the states to wear the proper mask at the appropriate times.
We invite you to subscribe to this channel and the realeverything.com and thepaleomom.com blogs and newsletters.
If you haven’t joined the Patreon family yet, head over for exclusive behind-the-scenes content about how Stacy and Sarah really feel about the topics they discuss. Your subscription goes to support this show and gets you direct access to Stacy and Sarah.
Thank you so much for listening, and we’ll see you next week!
Want more info on our Real Life? Healthy recipes, parenting tips, and general lifestyle stuff goes out in our Real Everything newsletter, join here.
Never want to miss a post, sale, or deal? Join my Healthy Inside & Out e-mail list for more info on non-toxic living and safer skincare!